Have you ever wondered how your doctor knows exactly where to place a joint injection for maximum effect, especially if they can’t see directly inside your joint? It’s a common question, and understanding the different approaches to joint injections can significantly impact your treatment outcome.
The Challenge of Traditional “Blind” Injections
For many common joint injections, the traditional method relies on the practitioner feeling for anatomical landmarks to guide the needle – essentially, making an educated guess about where the needle tip is going. While these “blind” techniques are often performed by skilled and experienced healthcare providers, they carry an inherent level of uncertainty.
Respected medical journals, including The Journal of Bone and Joint Surgery, have published studies highlighting the potential for inaccuracy with these blind injections. Research indicates that, depending on the specific joint and the technique used, a notable percentage of blind injections – sometimes around 25-30% or even higher for certain approaches – may not reach the intended target within the joint space. When medication isn’t delivered precisely where it’s needed most, the injection might be less effective in relieving pain, or could potentially lead to unnecessary discomfort or side effects.
The Arthritis Relief & Vascular Centers Difference: Precision Guidance
At Arthritis Relief & Vascular Centers (ARVC), we believe that when it comes to your joint health, guesswork simply has no place in your treatment plan. That’s why, particularly for patients with challenging anatomy, joint deformity, or advanced arthritis like significant osteoarthritis, our joint injections are guided by advanced imaging technology to ensure precise placement.
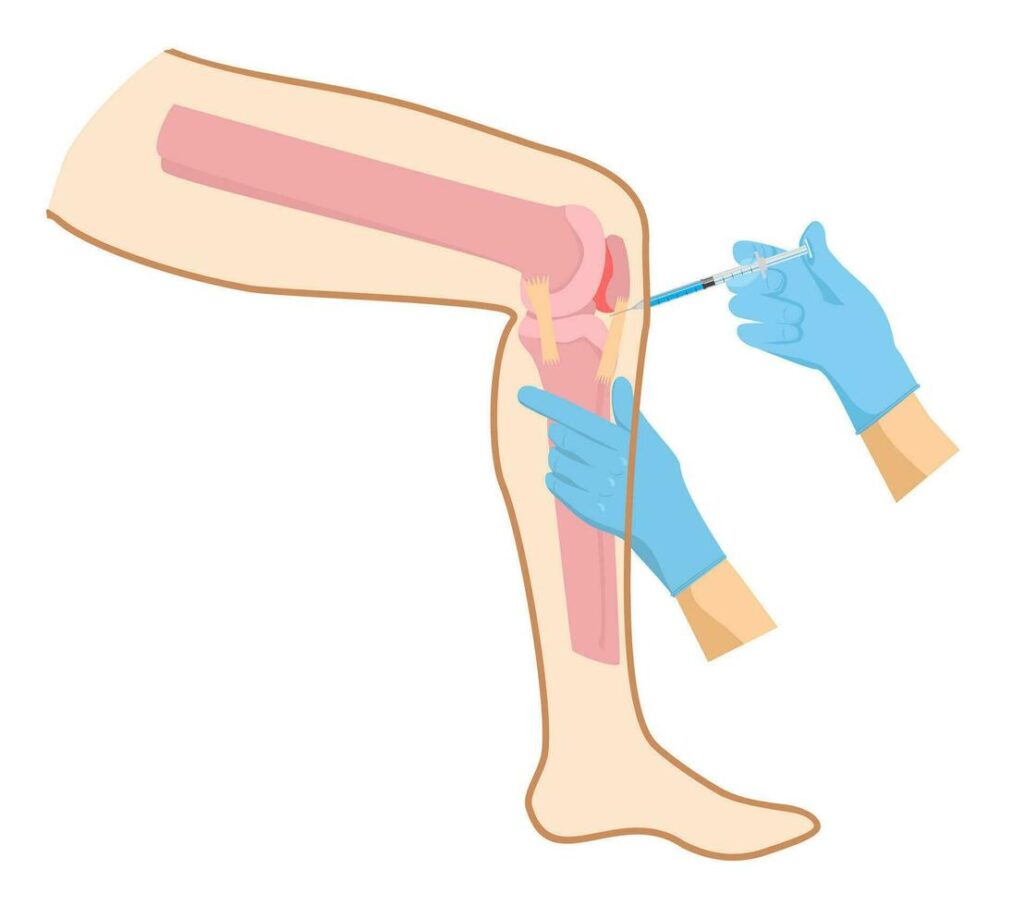
We utilize fluoroscopy, a specialized low-dose digital X-ray system. This technology allows our experienced physicians to see inside your joint in real-time throughout the injection procedure. Imagine it as having a live, internal map directing the medication with pinpoint accuracy to the very source of your pain.

Key Advantages of Fluoroscopic Guidance
This commitment to fluoroscopic guidance offers several crucial benefits for our patients:
- Maximum Effectiveness: By visualizing the needle tip’s exact path, we ensure accuracy in delivering medication directly into the targeted joint space or area. This precise placement is critical for achieving the best possible therapeutic outcome and optimal pain relief.
- Enhanced Safety: Real-time imaging allows our physicians to see internal structures and carefully navigate away from sensitive tissues like nerves and blood vessels. This significantly reduces the risk of adverse events or complications when compared to blind injection techniques.
- Improved Comfort: Accurate placement often translates to a smoother, more comfortable procedure for the patient.
- No Guesswork: With fluoroscopic guidance, the uncertainty inherent in blind injections is eliminated. We confirm the correct needle location before any medication is administered, ensuring your treatment is optimized for success right from the start.
Why Guided Imaging is Crucial, Especially for Osteoarthritis
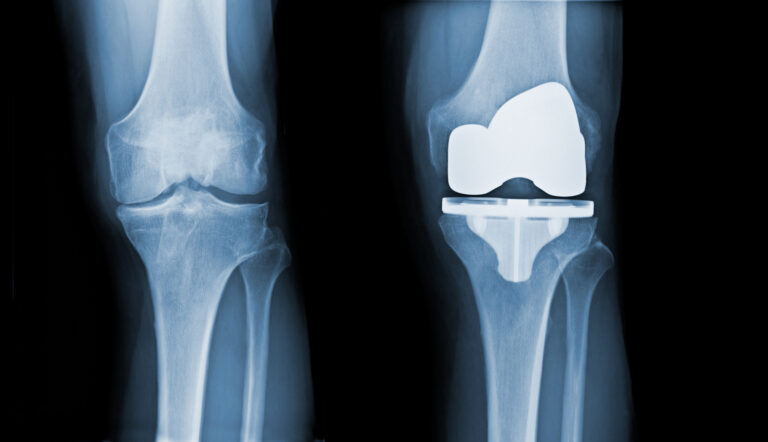
Patients dealing with significant osteoarthritis often present unique anatomical challenges that can make traditional joint injections less predictable. Consider conditions such as:
• Advanced Arthritis & Joint Space Narrowing: In these cases, the natural target area within the joint can be significantly reduced or physically altered.
• Bone Spurs (Osteophytes): These bony growths can obstruct the needle’s path or make landmark-based injection techniques difficult and less accurate.
• Joint Deformity: When a joint’s anatomy is no longer ‘standard’ due to arthritic changes, blind injections become much less reliable.
• Challenging Anatomy: Factors such as being overweight or the presence of joint effusion (fluid buildup) can further obscure anatomical landmarks, making it more difficult to accurately access the joint space without guidance.
In these common situations, the risk of a ‘blind’ injection missing the intended target within the joint is considerably greater. Fluoroscopic guidance empowers our physicians to navigate these complexities effectively in real-time. This ensures that the medication is delivered precisely to the narrowed or altered joint space, which is paramount for maximizing potential pain relief and minimizing discomfort for our patients with advanced osteoarthritis and other anatomical challenges.
Our commitment to using image guidance whenever clinically indicated, especially in cases of significant osteoarthritis or other anatomical challenges, reflects our dedication to providing the safest, most comfortable, and most effective care possible.
Learn More
To discover more about the advanced, non-surgical approaches to arthritis relief offered at Arthritis Relief & Vascular Centers, please visit us at www.arvcenters.com or call us at 210-899-0384 to schedule a consultation.
Disclaimer: The information in this blog post is for general informational purposes only and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.