A comprehensive guide to understanding and treating chronic pain after knee replacement surgery
Published by ARVCenters Author: Dr. Kevin S. Barton, DC Date: June 2025
Introduction: When Hope Meets Reality
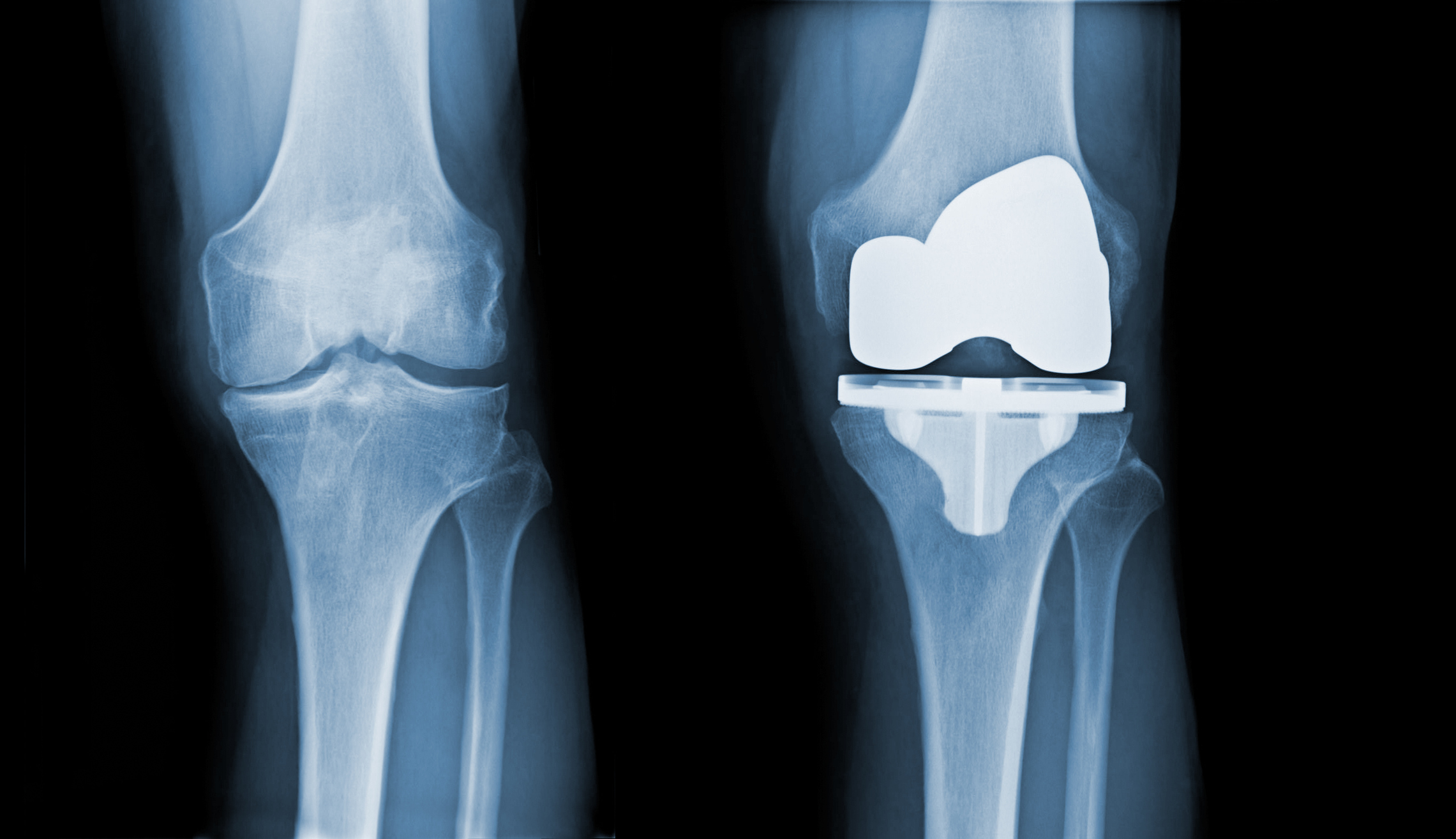
You did everything right. You endured months of worsening knee pain, tried physical therapy, conservative treatments, and pain medications. When these non-surgical approaches failed, you made the difficult decision to undergo knee replacement surgery. You followed your surgeon’s instructions, attended physical therapy sessions, and waited patiently for the promised relief. Yet here you are, months or even years later, still experiencing significant knee pain.
If this scenario sounds familiar, you are not alone. Despite the remarkable success of total knee arthroplasty (TKA) for most patients, approximately 20% continue to experience chronic pain after their procedure [1]. This translates to roughly 20,000 patients annually in the United States who find themselves in the frustrating position of having undergone major surgery only to face ongoing discomfort and functional limitations.
The emotional toll of persistent post-surgical pain cannot be understated. Patients often describe feelings of disappointment, frustration, and even betrayal by their own bodies. Many wonder if they made the wrong decision or if something went wrong during surgery. The reality is that chronic pain after knee replacement is a complex, multifaceted problem that can occur even when the surgery itself was technically perfect.
This comprehensive guide will explore the various reasons why pain may persist after knee replacement surgery, with particular focus on inflammation of the surrounding tissues and how innovative treatments like Genicular Artery Embolization (GAE) may offer new hope for those who have exhausted traditional options. We will examine the diagnostic process, treatment alternatives, and provide actionable information for patients who feel they have run out of options.
Understanding Chronic Pain After Knee Replacement
Defining the Problem
Chronic pain after total knee arthroplasty is medically defined as pain that persists for three to six months or longer following surgery [2]. This pain is distinct from the expected acute post-operative discomfort that gradually resolves during the normal healing process. Instead, chronic post-surgical pain is characterized by its persistence, often accompanied by functional limitations that significantly impact quality of life.
The International Association for the Study of Pain (IASP) recognizes chronic post-surgical pain as a distinct medical condition that develops or increases in intensity after a surgical procedure and significantly affects health-related quality of life [3]. In the context of knee replacement, this pain typically plateaus between three to six months after surgery, making it clear that the discomfort is not part of the normal recovery process.
The Scope of the Problem
Research consistently shows that chronic pain after knee replacement affects a substantial portion of patients. In a comprehensive systematic review of prospective studies, between 10% and 34% of patients reported unfavorable pain outcomes at follow-up periods ranging from three months to five years after surgery [4]. High-quality studies with multiple centers and low losses to follow-up have found that approximately 20% of patients report unfavorable pain outcomes at six months post-surgery [5].
More recent cohort studies have confirmed these findings, with 16% to 33% of patients reporting chronic pain after TKA [6]. Given that nearly 100,000 primary knee replacement operations are performed annually in the United Kingdom alone, and over 790,000 in the United States, the number of patients affected by this condition is substantial and growing [7].
The Impact on Patients’ Lives
Chronic pain after knee replacement extends far beyond physical discomfort. Research has demonstrated that this condition affects all dimensions of health-related quality of life, creating a cascade of problems that can fundamentally alter a patient’s daily existence [8].
Physical Impact
The physical consequences of persistent knee pain are multifaceted. Patients frequently experience functional limitations that restrict their ability to perform activities of daily living. Simple tasks such as climbing stairs, walking for extended periods, or getting up from a seated position can become challenging or impossible. The pain often leads to compensatory movement patterns that can create secondary problems in other joints, particularly the hip and ankle on the affected side, as well as the opposite knee.
Sleep disturbances are common, as patients struggle to find comfortable positions and may be awakened by pain during position changes. This sleep disruption creates a vicious cycle, as poor sleep quality can lower pain thresholds and increase pain sensitivity, making the original knee pain feel worse.
Psychological and Emotional Impact
The psychological impact of chronic pain after knee replacement is profound and often underestimated. Patients frequently experience depression and anxiety, particularly when they compare their current state to their pre-surgical expectations [9]. The disappointment of undergoing major surgery without achieving the anticipated relief can lead to feelings of hopelessness and despair.
Pain-related distress is often highest in those who experience no change or deterioration in pain symptoms following surgery [10]. Many patients report feeling betrayed by the medical system or questioning their decision to undergo surgery. This psychological burden can be particularly heavy for patients who delayed surgery for years, enduring progressive pain and functional decline, only to find themselves still in pain after the procedure.

Social and Economic Consequences
Chronic pain after knee replacement can lead to social isolation as patients withdraw from activities they once enjoyed. Relationships may suffer as patients become less able to participate in social gatherings, recreational activities, or family events. The inability to maintain previous levels of activity can lead to a sense of lost identity, particularly for individuals who were previously active or athletic.
The economic impact extends beyond the initial surgical costs. Patients with chronic pain often require ongoing medical care, including additional physician visits, imaging studies, medications, and sometimes revision surgeries. Lost productivity due to missed work days or early retirement can create significant financial strain. In the United Kingdom, chronic pain management accounts for 4.6 million general practitioner appointments per year at a cost of approximately £69 million [11].
Long-term Opioid Use and Dependency
One of the most concerning consequences of chronic pain after knee replacement is the potential for long-term opioid use. Patients who continue to experience significant pain may become dependent on opioid medications for pain management, creating additional health risks and complications. The opioid crisis has highlighted the importance of finding effective non-opioid treatments for chronic pain conditions, making innovative approaches like GAE increasingly valuable.
The Complex Causes of Persistent Pain After Knee Replacement
A Multifactorial Problem
Understanding why pain persists after knee replacement requires recognizing that this is rarely due to a single cause. Instead, chronic post-surgical pain typically results from a complex interplay of biological, surgical, and psychosocial factors [12]. This multifactorial nature explains why some patients experience excellent outcomes while others continue to struggle with pain despite having seemingly identical procedures.
The causes of chronic pain after TKA can be broadly categorized into several groups: mechanical factors related to the implant or surgical technique, biological factors including inflammation and nerve sensitization, and patient-specific factors such as genetics and psychological predisposition. Research has shown that the causes are not yet fully understood, although scientific interest in this area is rapidly growing [13].
Mechanical Causes
Implant-Related Issues
While modern knee replacement implants are highly sophisticated and generally very successful, mechanical problems can occasionally contribute to persistent pain. Implant loosening, though more commonly a cause of pain years or decades after surgery, can sometimes occur earlier and lead to chronic discomfort. Component malposition, where the artificial joint components are not optimally aligned, can create abnormal stress patterns and ongoing pain.
Instability of the knee joint due to inadequate soft tissue balancing during surgery can result in a feeling that the knee is “giving way” and can contribute to chronic pain. Patellar (kneecap) problems, including maltracking or anterior knee pain syndrome, are particularly common sources of persistent discomfort after knee replacement.
Altered Biomechanics
Total knee replacement fundamentally changes the biomechanics of the knee joint. While these changes are generally beneficial, some patients may experience difficulty adapting to the new joint mechanics. The artificial joint may not perfectly replicate the complex motion patterns of the natural knee, leading to altered gait patterns and compensatory movements that can contribute to ongoing discomfort.
Research has shown that post-TKA pain can be attributed to modified kinematics, alteration of ligament tensions, and increased retropatellar pressure [14]. These biomechanical changes can create stress on surrounding tissues and contribute to the development of chronic pain.
Inflammatory Causes: The Hidden Culprit
Understanding Post-Surgical Inflammation
One of the most significant and often overlooked causes of persistent pain after knee replacement is ongoing inflammation of the tissues surrounding the artificial joint. This inflammation can occur in several forms and locations, each contributing to the patient’s overall pain experience.
Synovitis, or inflammation of the synovial membrane that lines the joint, is increasingly recognized as a major contributor to chronic pain after knee replacement [15]. The synovial membrane produces synovial fluid that lubricates the joint, but when inflamed, it can become thickened and produce excess fluid, leading to joint swelling and pain. Studies have shown that chronic pain correlates with synovitis at one and two years post-surgery, highlighting the persistent nature of this inflammatory process [16].
The Role of Abnormal Blood Vessel Growth
A key mechanism underlying persistent inflammation is the development of abnormal blood vessels (neovascularization also known as angiogenesis) in and around the knee joint. These abnormal blood vessels, which can grow into bone and soft tissues, become inflamed and compressed, directly contributing to pain and swelling. This process is similar to what occurs in osteoarthritis, where abnormal blood vessel growth is associated with pain and disease progression.
The genicular arteries, which supply blood to the knee joint including bones, ligaments, tendons, and muscles, play a crucial role in this process. In patients with persistent pain, these arteries may develop abnormal branching patterns and increased blood flow to inflamed tissues. This hypervascularity creates a cycle where increased blood flow leads to more inflammation, which in turn stimulates further blood vessel growth.
Inflammatory Mediators and Pain Sensitization
Chronic inflammation after knee replacement involves the release of various inflammatory mediators, including cytokines, prostaglandins, and other pain-producing substances. These mediators not only cause direct tissue damage but also sensitize pain receptors, making the knee more sensitive to painful stimuli. This sensitization can explain why some patients experience pain that seems disproportionate to any visible structural problems.
The inflammatory process can also affect nerve function, leading to neuropathic pain characteristics such as burning, tingling, or electric shock-like sensations. This type of pain is often more difficult to treat with traditional pain medications and may require specialized approaches.
Nerve-Related Causes
Peripheral Nerve Injury
Surgical trauma during knee replacement can occasionally result in injury to peripheral nerves around the knee. The most commonly affected nerves include the saphenous nerve, which provides sensation to the inner aspect of the knee and lower leg, and branches of the peroneal nerve, which can affect sensation and function in the foot and ankle.
Nerve damage can manifest as numbness, tingling, burning pain, or loss of function. In some cases, patients may develop complex regional pain syndrome (CRPS), a condition characterized by severe, burning pain that is often accompanied by changes in skin color, temperature, and sweating patterns.
Central Sensitization
Prolonged pain signals from the knee can lead to changes in the central nervous system’s processing of pain information. This phenomenon, known as central sensitization, can result in amplification of pain signals and the development of pain in response to normally non-painful stimuli. Central sensitization helps explain why some patients continue to experience pain even when local tissue healing appears complete.
Infection: The Great Mimicker
Subclinical Infection
While obvious infections after knee replacement are typically identified and treated promptly, subclinical or low-grade infections can be much more difficult to diagnose. These infections may not cause the classic signs of redness, warmth, and fever, but can still contribute to persistent pain and inflammation.
Biofilm formation on the artificial joint components can harbor bacteria that are resistant to both the immune system and antibiotics. These biofilms can maintain a low-level inflammatory state that contributes to ongoing pain without causing obvious signs of infection.
Diagnostic Challenges
Diagnosing subclinical infection requires specialized testing, including analysis of joint fluid for inflammatory markers and bacterial cultures. Advanced imaging techniques and sometimes tissue biopsies may be necessary to identify these hidden infections. The challenge is that many of the symptoms of subclinical infection overlap with other causes of persistent pain, making diagnosis difficult.
Patient-Specific Risk Factors
Preoperative Factors
Several factors present before surgery can increase the risk of developing chronic pain after knee replacement. Patients with higher levels of preoperative pain, particularly those with central sensitization or widespread pain conditions, are at increased risk. Psychological factors such as depression, anxiety, and catastrophic thinking patterns can also predispose patients to poor pain outcomes.
Genetic factors may play a role, as some individuals appear to be more susceptible to developing chronic pain conditions. Research is ongoing to identify specific genetic markers that might predict which patients are at highest risk for persistent pain after surgery.
Surgical and Postoperative Factors
Factors during and immediately after surgery can also influence long-term pain outcomes. Inadequate pain control in the immediate postoperative period may contribute to the development of chronic pain through sensitization mechanisms. Complications during surgery, prolonged operative time, or technical difficulties can increase the risk of persistent pain.
The rehabilitation process is also crucial. Patients who experience complications during physical therapy, develop scar tissue formation, or have difficulty regaining range of motion may be at higher risk for chronic pain. Conversely, patients who achieve good functional outcomes are less likely to experience persistent pain.
Genicular Artery Embolization: A Revolutionary Treatment Approach
Introduction to GAE
For patients experiencing persistent pain after knee replacement surgery, particularly when inflammation and abnormal blood vessel growth are contributing factors, Genicular Artery Embolization (GAE) represents a groundbreaking treatment option. This innovative, minimally invasive procedure offers new hope for individuals who have exhausted traditional treatment options without finding adequate relief.
GAE is a novel interventional radiology procedure that specifically targets the abnormal blood vessels contributing to knee pain and inflammation. Unlike traditional treatments that often provide only temporary relief or require major surgical intervention, GAE addresses the underlying vascular abnormalities that perpetuate the inflammatory cycle responsible for persistent pain.
Understanding the Science Behind GAE
The Vascular Component of Knee Pain
To understand how GAE works, it’s essential to recognize the role that blood vessels play in knee pain, particularly in the context of persistent inflammation after joint replacement. The knee joint is supplied by seven genicular arteries that provide blood to the bones, ligaments, tendons, and muscles in the area. Under normal circumstances, these arteries maintain healthy blood flow to support joint function and healing.
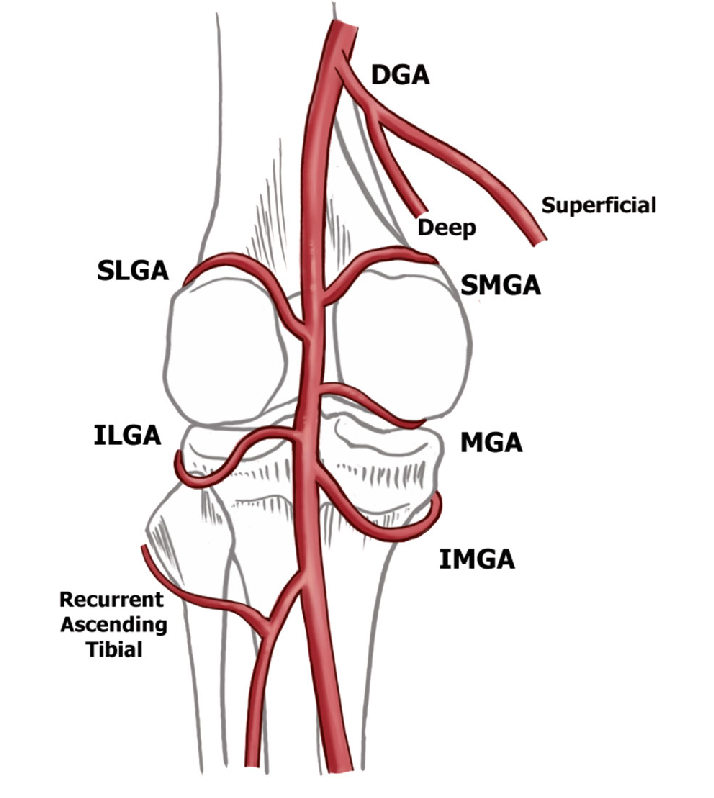
However, in patients with persistent pain after knee replacement, these genicular arteries often develop abnormal characteristics. They may become enlarged, develop excessive branching patterns, or create new blood vessels (neovascularization) that grow into areas where they don’t belong. This abnormal vascular growth is often associated with inflammation and can directly contribute to pain generation.
Targeting Abnormal Vascularity
GAE works by identifying and selectively blocking these abnormal blood vessels while preserving normal blood flow to healthy tissues. The procedure targets what radiologists call “tumor blush-type enhancement” – areas of abnormal blood vessel growth that appear as bright spots on specialized imaging studies and correspond to areas of knee pain or tenderness.
By reducing blood flow to these inflamed and abnormal areas, GAE can break the cycle of inflammation that perpetuates pain. The procedure is hypothesized to reduce knee pain through several mechanisms: reducing inflammation, decreasing abnormal blood vessel growth (neovascularization), and interrupting the formation of new nerve pathways (neoinnervation) that contribute to pain sensation [17].
The GAE Procedure: What Patients Can Expect
Pre-Procedure Evaluation
Before undergoing GAE, patients undergo a comprehensive evaluation to determine if they are appropriate candidates for the procedure. This evaluation typically includes a detailed medical history, physical examination, and specialized imaging studies to identify the source of pain and confirm the presence of abnormal blood vessels.
CT imaging may be used to assess for signs of inflammation, bone changes, or other complications around the knee joint. In some cases, diagnostic angiography may be performed to visualize the genicular arteries and identify areas of abnormal blood flow. This thorough evaluation helps ensure that GAE is likely to be beneficial for each individual patient.
The Procedure Itself
GAE is performed as an outpatient procedure, typically taking approximately one hour to complete. The procedure is performed by an interventional radiologist, a physician specially trained in minimally invasive, image-guided procedures.
The patient is positioned comfortably on an examination table, and the procedure is performed under local anesthesia with conscious sedation for comfort. A small incision, typically less than 3 millimeters, is made in the groin area to access the femoral artery. Through this tiny incision, a thin, flexible catheter (tube) is inserted and guided through the blood vessels to reach the genicular arteries supplying the knee.
Using real-time X-ray guidance (fluoroscopy), the interventional radiologist carefully navigates the catheter to the specific genicular arteries that are contributing to the patient’s pain. Contrast dye is injected to visualize the blood vessels and identify areas of abnormal blood flow or “blush” that correspond to the patient’s pain.
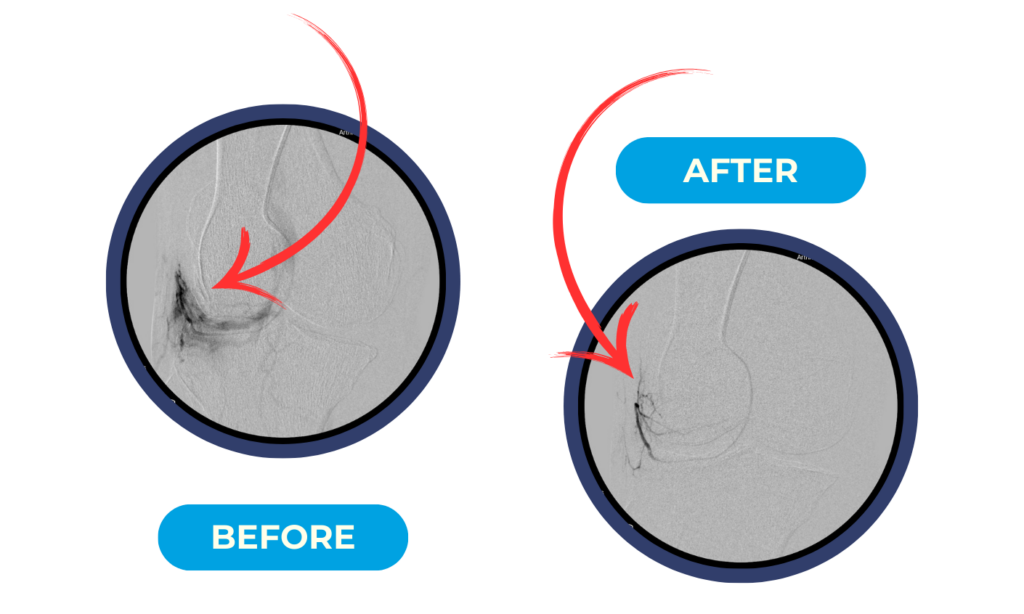
Once the abnormal blood vessels are identified, tiny particles called embolic agents are injected through the catheter directly into these vessels. These particles, which are smaller than the width of a human hair, block blood flow to the abnormal vessels while preserving circulation to healthy tissues. The most commonly used embolic agents are microspheres, which are biocompatible and permanent.
Immediate Post-Procedure Care
After the procedure, patients are monitored for several hours to ensure there are no immediate complications. The small incision in the groin is closed with a simple bandage, and patients can typically walk within a few hours. Most patients are discharged the same day and can return to normal activities within 24 to 48 hours.
Pain relief from GAE is typically gradual, with most patients beginning to notice improvement within a few weeks of the procedure. Maximum benefit is usually achieved within 1 to 3 months, as the inflammatory process subsides and the abnormal blood vessels are permanently blocked.

Clinical Evidence and Effectiveness
Research Results
The clinical evidence supporting GAE for knee pain continues to grow, with multiple studies demonstrating its safety and effectiveness. A comprehensive meta-analysis of GAE studies found impressive results that offer hope for patients with persistent knee pain [18].
In this analysis of 270 patients across 9 studies, GAE demonstrated a technical success rate of 99.7%, meaning that the procedure could be completed successfully in virtually all patients. Over a 12-month follow-up period, patients experienced significant improvements in pain scores, with visual analog scale (VAS) pain scores improving by 34 to 39 points on a 100-point scale. Similarly, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores, which measure pain and function, improved by 28 to 34 points.
Clinically Meaningful Outcomes
Perhaps more importantly than statistical significance, these improvements represent clinically meaningful changes in patients’ lives. At 12 months after GAE, 78% of patients met the minimal clinically important difference (MCID) for pain relief, meaning they experienced a level of improvement that was noticeable and meaningful in their daily lives. An impressive 92% of patients met the MCID for overall knee function, and 78% achieved what researchers call “substantial clinical benefit” – a level of improvement that represents a major positive change in quality of life.
Factors Predicting Success
Research has identified several factors that may predict which patients are most likely to benefit from GAE. Patients with higher baseline pain severity tend to experience greater improvements, suggesting that GAE may be particularly beneficial for those with severe, persistent pain. This finding is encouraging for patients who have been struggling with significant discomfort after knee replacement surgery.
Long-term Outcomes
Long-term follow-up data shows that the benefits of GAE are durable. Over a two-year period, only 5.2% of patients who underwent GAE subsequently required total knee replacement surgery, and 8.3% received repeat GAE procedures. This suggests that for most patients, a single GAE procedure provides lasting relief.
Safety Profile and Risks
Excellent Safety Record
One of the most attractive aspects of GAE is its excellent safety profile. The procedure is minimally invasive, performed through a tiny incision, and does not require general anesthesia. This makes it suitable for patients who may not be candidates for more invasive surgical procedures due to medical comorbidities or advanced age.
Minor and Temporary Side Effects
The most common side effect of GAE is transient skin discoloration, which occurs in approximately 11.6% of patients [19]. This discoloration typically appears as a temporary darkening or bruising of the skin around the knee and resolves completely within a few weeks. Other minor side effects may include temporary swelling or mild discomfort at the procedure site.
Serious Complications Are Rare
Serious complications from GAE are extremely rare. Because the procedure specifically targets abnormal blood vessels while preserving normal circulation, the risk of compromising healthy tissue is minimal. The embolic particles used are biocompatible and do not cause adverse reactions in the body.
Comparison to Surgical Alternatives
When compared to more invasive surgical options such as revision knee replacement, GAE offers a much more favorable risk-benefit profile. Revision surgery carries significant risks including infection, blood clots, nerve damage, and prolonged recovery periods. GAE, in contrast, allows patients to return to normal activities within days rather than months.
GAE for Post-Surgical Knee Pain: A Targeted Approach
Addressing Post-Replacement Inflammation
While most GAE research has focused on patients with osteoarthritis who have not undergone knee replacement, the principles underlying the procedure make it highly relevant for patients with persistent pain after joint replacement surgery. The inflammatory processes that GAE targets – abnormal blood vessel growth, synovitis, and tissue inflammation – can occur around artificial joints just as they do in native joints.In our practice at ARVCenters, roughly 1 in 15 GAE patients are patients with persistent pain after knee replacement surgery.
In fact, patients with persistent pain after knee replacement are ideal candidates for GAE because the procedure can address the inflammatory component of their pain without interfering with the artificial joint itself. Unlike revision surgery, which requires removing and replacing the artificial joint components, GAE works by targeting the soft tissues and blood vessels around the joint.
Breaking the Inflammatory Cycle
For patients with post-surgical pain, GAE offers the opportunity to break the cycle of inflammation that may be perpetuating their discomfort. By reducing blood flow to inflamed tissues and abnormal blood vessels, GAE can allow the inflammatory process to resolve, potentially providing significant pain relief without the need for additional major surgery.
Complementary to Other Treatments
GAE can be used in combination with other treatments for post-surgical knee pain. Patients can continue with physical therapy, anti-inflammatory medications, and other conservative treatments while undergoing GAE. The procedure does not preclude future treatments, including revision surgery if ultimately necessary.
Patient Selection and Candidacy
Ideal Candidates for GAE
The ideal candidate for GAE in the context of post-surgical knee pain is a patient who continues to experience significant discomfort despite having a well-functioning artificial joint. These patients typically have evidence of ongoing inflammation around the knee, which may be detected through physical examination, imaging studies, or laboratory tests.
Candidates for GAE generally share several characteristics:
•Persistent knee pain lasting more than 12 months after knee replacement surgery
•Pain that interferes with daily activities and quality of life
•Evidence of inflammation around the knee joint
•Failure to achieve adequate relief with conservative treatments
•Absence of obvious mechanical problems with the artificial joint
•Good overall health status to undergo the procedure
Diagnostic Workup
Before considering GAE, patients undergo a thorough diagnostic evaluation to identify the source of their persistent pain. This evaluation may include advanced imaging studies such as MRI to assess for synovitis, bone scans to evaluate for loosening or infection, and sometimes joint aspiration to analyze synovial fluid.
The goal of this diagnostic workup is to confirm that inflammation is a significant component of the patient’s pain and to rule out other causes that might require different treatments. Patients with evidence of implant loosening, infection, or significant mechanical problems may not be appropriate candidates for GAE and may require surgical intervention instead.
Contraindications and Limitations
While GAE is suitable for many patients with persistent post-surgical knee pain, there are some contraindications and limitations to consider. Patients with active infection around the knee joint should have the infection treated before considering GAE. Those with severe kidney disease may not be able to receive the contrast dye used during the procedure.
Patients with significant mechanical problems with their artificial joint, such as loosening or instability, may not benefit from GAE alone and may require surgical revision.
The Diagnostic Journey: Identifying the Source of Persistent Pain
The Importance of Accurate Diagnosis
For patients experiencing persistent pain after knee replacement surgery, obtaining an accurate diagnosis is crucial for developing an effective treatment plan. The diagnostic process can be complex because multiple factors may contribute to ongoing pain, and symptoms can overlap between different conditions. A systematic approach to diagnosis helps ensure that patients receive the most appropriate treatment for their specific situation.
The diagnostic journey typically begins with a comprehensive history and physical examination, followed by targeted imaging studies and laboratory tests as needed. The goal is not only to identify what is causing the pain but also to rule out serious conditions that require immediate attention, such as infection or implant failure.
Clinical Evaluation
Detailed History Taking The diagnostic process begins with a thorough discussion of the patient’s symptoms, including the character, location, timing, and severity of pain. Healthcare providers will ask about factors that worsen or improve the pain, associated symptoms such as swelling or stiffness, and how the pain affects daily activities and sleep.
Understanding the timeline of pain is particularly important. Pain that has been present since surgery may suggest different causes than pain that developed months or years later. The relationship between pain and activity levels, weather changes, and other factors can provide valuable clues about the underlying cause.
Physical Examination A comprehensive physical examination focuses on assessing the knee joint and surrounding structures. The examiner will look for signs of inflammation such as swelling, warmth, or redness around the knee. Range of motion testing helps identify stiffness or mechanical limitations that might contribute to pain.
Palpation of the knee can help localize areas of tenderness and identify specific structures that may be involved in the pain process. Special tests may be performed to assess the stability of the artificial joint and evaluate the function of surrounding muscles and ligaments.
Advanced Imaging Studies
Magnetic Resonance Imaging (MRI) MRI is particularly valuable for evaluating soft tissue structures around the knee replacement. Specialized MRI techniques can be used to assess for synovitis, fluid collections, and other inflammatory changes that might not be visible on standard X-rays. Metal artifact reduction sequences allow for better visualization of tissues around the artificial joint components.
MRI can also help identify complications such as component loosening, osteolysis (bone destruction), or soft tissue masses that might contribute to pain. In some cases, MRI findings can help determine whether a patient might benefit from GAE by identifying areas of inflammation and abnormal tissue enhancement.
Nuclear Medicine Studies Bone scans and other nuclear medicine studies can provide information about bone metabolism and blood flow around the artificial joint. These studies can help identify areas of increased bone turnover that might indicate loosening, infection, or other complications.
Three-phase bone scans can be particularly useful for distinguishing between different causes of persistent pain. Patterns of uptake on these scans can help differentiate between mechanical loosening, infection, and inflammatory conditions.
Laboratory Testing
Inflammatory Markers
Blood tests can provide valuable information about the presence and severity of inflammation in the body. Tests such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) can be elevated in patients with ongoing inflammation, though these tests are not specific to the knee joint.
More specific markers of inflammation may be measured in some cases, including cytokines and other inflammatory mediators that can provide insight into the underlying inflammatory processes contributing to pain.
Joint Fluid Analysis
In some cases, fluid may be aspirated from the knee joint for analysis. This fluid can be tested for signs of infection, including bacterial cultures and white blood cell counts. Crystal analysis can help identify conditions such as gout or pseudogout that might contribute to pain and inflammation.
The presence of metal particles or other debris in the joint fluid can provide evidence of implant wear or other mechanical problems that might require surgical intervention.
Ruling Out Serious Complications
Infection Detection
One of the most important aspects of the diagnostic workup is ruling out infection around the artificial joint. Prosthetic joint infections can be challenging to diagnose because they may not always cause obvious symptoms such as fever or visible signs of infection.
Advanced diagnostic techniques may be needed to identify subtle infections, including specialized imaging studies, joint fluid analysis, and sometimes tissue biopsies. Early detection and treatment of infection is crucial because untreated prosthetic joint infections can lead to serious complications and may require removal of the artificial joint.
Implant Assessment
The diagnostic workup must also assess the integrity and function of the artificial joint components. X-rays are typically the first step in evaluating implant position and stability. Signs of loosening, wear, or component migration can indicate mechanical problems that require surgical intervention.
Advanced imaging techniques such as CT scans or specialized X-ray views may be needed to fully assess implant function. In some cases, the artificial joint may appear normal on imaging studies despite causing pain, making diagnosis more challenging.
Alternative Treatment Options: A Comprehensive Approach
Conservative Management Strategies
Medication Management
For patients with persistent pain after knee replacement, medication management often forms the foundation of treatment. However, the approach to pain medication in this population requires careful consideration of the underlying causes of pain and the potential for long-term medication use.
Non-steroidal anti-inflammatory drugs (NSAIDs) can be effective for patients whose pain has a significant inflammatory component. These medications work by reducing inflammation and can provide meaningful pain relief for some patients. However, long-term use of NSAIDs carries risks including gastrointestinal bleeding, kidney problems, and cardiovascular complications, particularly in older adults.
Topical anti-inflammatory preparations may provide some benefit with fewer systemic side effects than oral medications. These preparations can be applied directly to the skin over the painful area and may help reduce local inflammation.
For patients with neuropathic pain characteristics, medications such as gabapentin or pregabalin may be beneficial. These medications work by modulating nerve signal transmission and can be particularly effective for burning, tingling, or electric shock-like pain.
Physical Therapy and Rehabilitation
Continued physical therapy can be beneficial for patients with persistent pain after knee replacement, even years after surgery. A skilled physical therapist can identify movement patterns that may be contributing to pain and develop targeted exercises to address these issues.
Specific techniques that may be helpful include manual therapy to address soft tissue restrictions, strengthening exercises for muscles around the knee and hip, and gait training to optimize walking patterns. Aquatic therapy can be particularly beneficial because the buoyancy of water reduces stress on the joint while allowing for movement and exercise.
Important Considerations Regarding Injection Therapies
For patients with knee replacements, injection therapies into or around the artificial joint carry significant risks that must be carefully considered. The presence of an artificial joint creates a unique environment where any introduction of bacteria through injection procedures can lead to serious prosthetic joint infections.
Prosthetic joint infections are among the most serious complications that can occur after knee replacement surgery. These infections can be devastating, often requiring removal of the artificial joint, prolonged antibiotic treatment, and multiple revision surgeries. The risk of infection from injection procedures, while relatively low, is significantly higher in patients with artificial joints compared to those with natural joints.
For this reason, many orthopedic surgeons and infectious disease specialists strongly advise against injection therapies directly into or around knee replacements. The potential temporary pain relief from injections is generally considered to outweigh the serious risks of introducing infection to the artificial joint.
Patients with persistent pain after knee replacement should discuss these risks thoroughly with their healthcare providers. Alternative pain management strategies that do not involve injection into the joint space, such as oral medications, topical treatments, and innovative procedures like GAE, may be safer and more appropriate options for managing persistent pain in this population.
Interventional Pain Management
Nerve Blocks and Ablation
For patients whose pain has a significant nerve component, targeted nerve blocks or ablation procedures may provide relief. Genicular nerve blocks involve injecting local anesthetic around the nerves that supply sensation to the knee joint. If these blocks provide temporary
These procedures are minimally invasive and can be performed on an outpatient basis. While they don’t address the underlying cause of inflammation, they can provide significant pain relief for appropriately selected patients.
Spinal Cord Stimulation
For patients with severe, refractory pain that doesn’t respond to other treatments, spinal cord stimulation may be considered. This technique involves implanting a small device that delivers electrical impulses to the spinal cord, interrupting pain signals before they reach the brain.
While spinal cord stimulation is more invasive than other treatments, it can provide significant pain relief for patients who have exhausted other options. The procedure is reversible, and patients can undergo a trial period to determine if the treatment is effective before committing to permanent implantation.
Surgical Options
Revision Surgery
In some cases, revision surgery may be necessary to address persistent pain after knee replacement. This is typically considered when there is clear evidence of mechanical problems with the artificial joint, such as loosening, instability, or significant wear.
Revision surgery is more complex than primary knee replacement and carries higher risks of complications. Recovery time is typically longer, and outcomes may not be as predictable as with primary surgery. However, for patients with clear mechanical problems, revision surgery may be the most effective treatment option.
The Role of Multidisciplinary Care
Pain Management Specialists
Patients with persistent pain after knee replacement often benefit from evaluation by pain management specialists who have expertise in complex pain conditions. These specialists can provide comprehensive pain assessments and develop individualized treatment plans that may include multiple modalities.
Pain management specialists are also skilled in the use of interventional procedures such as nerve blocks and can help coordinate care with other specialists involved in the patient’s treatment.
Psychological Support
The psychological impact of persistent pain after knee replacement should not be underestimated. Patients may benefit from counseling or psychological support to help cope with chronic pain and its effects on quality of life.
Cognitive-behavioral therapy and other psychological interventions can help patients develop coping strategies and may actually help reduce pain perception. Some patients may benefit from treatment for depression or anxiety that has developed as a result of their chronic pain.
Integrative Approaches
Some patients find benefit from integrative approaches to pain management, including acupuncture, massage therapy, and mind-body techniques such as meditation or yoga. While the evidence for these approaches in post-surgical knee pain is limited, they are generally safe and may provide additional benefit when used alongside conventional treatments.
GAE vs. Traditional Treatments: A Comparative Analysis
Advantages of GAE
Minimally Invasive Nature
One of the primary advantages of GAE compared to traditional surgical treatments is its minimally invasive nature. While revision knee surgery requires a large incision, removal of existing implants, and extensive tissue dissection, GAE is performed through a tiny puncture in the groin that requires only a small bandage for closure.
This minimally invasive approach translates to several practical benefits for patients. Recovery time is measured in days rather than months, allowing patients to return to normal activities quickly. The risk of complications is significantly lower, and the procedure can be performed on an outpatient basis, eliminating the need for hospitalization.
Targeted Treatment Approach
GAE offers a targeted approach to treating the specific cause of pain – abnormal blood vessels and inflammation – rather than addressing symptoms alone. Traditional pain medications provide temporary relief but don’t address the underlying inflammatory process. GAE, in contrast, can provide lasting relief by permanently blocking the abnormal blood vessels that contribute to inflammation and pain.
This targeted approach means that GAE can be effective even when other treatments have failed. Patients who have not responded to medications, injections, or physical therapy may still benefit from GAE because it addresses a different aspect of their pain condition.
Preservation of Treatment Options
Unlike revision surgery, which is a major undertaking that may limit future treatment options, GAE preserves all other treatment possibilities. Patients who undergo GAE can still receive medications, injections, physical therapy, and even revision surgery if needed in the future.
This preservation of options is particularly important for patients who are not ready for major surgery or who want to try less invasive treatments first. GAE can serve as a bridge treatment that provides pain relief while patients consider their long-term treatment options.
Limitations and Considerations
Patient Selection
While GAE can be highly effective for appropriately selected patients, it is not suitable for everyone with persistent knee pain. Patients whose pain is primarily due to mechanical problems with the artificial joint, such as loosening or instability, are unlikely to benefit from GAE and may require surgical intervention.
Time to Benefit
Unlike some treatments that provide immediate relief, GAE typically requires several weeks to months to achieve maximum benefit. Patients need to understand that pain relief will be gradual and that they may not notice significant improvement immediately after the procedure.
This delayed onset of benefit can be challenging for patients who are seeking immediate relief from severe pain. However, the gradual improvement often leads to more durable and lasting pain relief compared to treatments that provide only temporary benefit.
Cost Considerations
Initial Procedure Costs
The cost of GAE is typically significantly lower than revision knee surgery when considering both the direct medical costs and indirect costs such as lost productivity and extended rehabilitation. GAE is performed on an outpatient basis, eliminating hospital stay costs, and the recovery period is much shorter.
Many insurance plans cover GAE for appropriate indications, though coverage policies may vary. Patients should check with their insurance providers to understand their specific coverage for this procedure.
Long-term Economic Benefits
When GAE is successful in providing lasting pain relief, it can result in significant long-term cost savings. Patients may require fewer medications, physician visits, and other treatments for their knee pain. The ability to return to normal activities more quickly can also reduce indirect costs related to lost productivity and disability.
For patients who would otherwise require revision surgery, GAE can potentially delay or eliminate the need for this more expensive and risky procedure. Even if revision surgery is eventually needed, GAE can provide a period of improved function and quality of life.
Patient Stories: Real Experiences with ARVCenters
The following testimonials are from actual ARVCenters patients who have shared their experiences through video testimonials. These stories represent real outcomes and provide hope for others facing similar challenges.
A Remarkable Journey: From 23 Surgeries to Relief
One of the most inspiring testimonials comes from our patient, Maggie who had endured an extraordinary medical journey before finding relief at ARV Centers. Having undergone 23 knee surgeries before the age of 60, this patient’s story represents the extreme end of surgical complications and persistent pain that can occur even with multiple interventions.
“I had 23 knee surgeries before I turned 60,” the patient shares in their video testimonial. “What happened next will surprise you.” This patient’s experience highlights how even those with the most complex surgical histories can find relief through innovative treatments like Genicular Artery Embolization.
The patient’s journey to ARVCenters came after decades of surgical interventions that failed to provide lasting relief. Their case demonstrates that GAE can be effective even for patients with extensive surgical histories and complex pain patterns. The procedure offered a non-surgical solution that could address the underlying inflammatory processes contributing to their persistent pain.
This testimonial is particularly relevant for patients who have undergone knee replacement surgery and continue to experience pain, as it shows that GAE can be effective for post-surgical pain management. The patient’s story serves as a beacon of hope for others who may feel they have exhausted all surgical options.
The success of this case underscores the importance of considering innovative treatments like GAE, especially for patients with complex medical histories who may not be candidates for additional surgical interventions. It demonstrates that even after multiple failed surgeries, effective pain relief may still be possible through targeted, minimally invasive procedures.

Dolores: Ten Years of Pain, Finally Resolved
Dolores’s story represents the journey of countless patients who suffer with chronic knee arthritis for years before finding effective treatment. Her testimonial, titled “How Dolores Fixed Her Knee Pain After 10 Years,” chronicles a decade-long struggle with knee pain that was finally resolved through treatment at ARV Centers.
Dolores’s experience highlights the progressive nature of knee arthritis and how it can gradually worsen over time, despite various treatment attempts. Her decade-long journey with pain illustrates the significant impact that chronic knee pain can have on quality of life, limiting daily activities and affecting overall well-being.
The turning point in Dolores’s story came when she discovered ARV Centers and learned about their non-surgical treatment options. “The team at ARV Centers took the time to really understand my condition and explain how their treatment could help,” she recalls. “For the first time in years, I felt hopeful.”
Dolores underwent treatment at ARV Centers and experienced remarkable improvement in her knee pain. “I can’t believe the difference,” she says. “After 10 years of constant pain, I finally have my life back. I can do the things I love again without being limited by knee pain.”
Her testimonial emphasizes the life-changing potential of appropriate treatment and the importance of not giving up hope, even after years of unsuccessful treatments. Dolores’s story demonstrates that effective relief is possible, even for long-standing cases of chronic knee pain.
From Pain Level 8 to Zero: A Personal Success Story
Perhaps one of the most compelling testimonials comes from a patient who experienced dramatic pain relief through GAE treatment at ARVCenters. In their video titled “Can This Fix Knee Pain Without Surgery?”, this patient shares their personal journey from severe pain to complete relief.
“Don’t let knee pain ruin your life for so many years,” the patient advises others in their testimonial. Speaking from personal experience, they describe how Genicular Artery Embolization at ARVCenters transformed their life. “GAE took my pain from an 8 to ZERO – just like it did for me!”
This testimonial is particularly powerful because it provides specific, measurable outcomes. The patient’s pain level dropped from 8 out of 10 – representing severe, life-limiting pain – to zero, indicating complete pain relief. This dramatic improvement demonstrates the potential effectiveness of GAE for appropriately selected patients.
The patient’s enthusiasm in sharing their story reflects the profound impact that effective pain treatment can have on a person’s life. “I wish I had known about this treatment sooner,” they reflect. “I could have avoided years of unnecessary suffering.”
This testimonial also emphasizes the non-surgical nature of the GAE procedure, which was particularly appealing to this patient. “I was hesitant about more surgery,” they explain. “But GAE is minimally invasive – it’s nothing like major surgery. The recovery was so much easier than I expected.”
The patient’s decision to share their story publicly demonstrates their commitment to helping others who may be suffering from similar pain. “If my story can help even one person avoid years of pain like I experienced, then sharing it is worth it,” they conclude.
Common Themes in Patient Experiences
Across all the ARVCenters patient testimonials, several common themes emerge that provide valuable insights for prospective patients:
Years of Unsuccessful Treatments
Many patients describe trying multiple treatments over years before finding relief at ARV Centers. This pattern highlights the complexity of chronic knee pain and the importance of specialized care from providers who understand advanced treatment options.
Life-Changing Results
Patients consistently describe their outcomes as “life-changing” and express gratitude for being able to return to activities they love. This emotional impact underscores the profound effect that chronic pain can have on quality of life and the equally profound relief that effective treatment can provide.
Minimally Invasive Approach
Patients appreciate the minimally invasive nature of GAE compared to surgical alternatives. The quick recovery time and outpatient nature of the procedure are frequently mentioned as significant advantages.
Hope for Others
Many patients express a desire to share their stories to help others who may be suffering from similar conditions. This altruistic motivation reflects the gratitude patients feel for their improved quality of life and their recognition of how difficult chronic pain can be.
Professional, Compassionate Care
Patients consistently praise the team at ARV Centers for their expertise, professionalism, and compassionate approach to care. The importance of feeling heard and understood by healthcare providers is a recurring theme in patient testimonials.
The Impact of Real Patient Stories
These authentic patient testimonials serve multiple important purposes for individuals considering treatment for persistent knee pain:
Realistic Expectations
Real patient stories provide realistic expectations about treatment outcomes, recovery times, and the patient experience. This helps prospective patients make informed decisions about their care.
Emotional Support
Hearing from others who have faced similar challenges can provide emotional support and reduce feelings of isolation that often accompany chronic pain conditions.
Treatment Validation
Patient testimonials provide real-world validation of treatment effectiveness beyond clinical studies and medical literature.
Inspiration and Hope
Success stories can inspire patients who may have lost hope after multiple failed treatments to consider new options and maintain optimism about their potential for improvement.
These testimonials from ARVCenters patients demonstrate that effective treatment for persistent knee pain is possible, even for complex cases with long histories of unsuccessful treatments. They provide hope and encouragement for others facing similar challenges while highlighting the importance of seeking care from specialists who understand advanced treatment options like GAE.
Hope and Next Steps: Moving Forward with Confidence
The Importance of Not Giving Up
For patients experiencing persistent pain after knee replacement surgery, it’s crucial to understand that effective treatment options are available. The development of GAE and other innovative treatments means that patients who have not found relief with traditional approaches now have new reasons for hope.
The key is to work with healthcare providers who understand the complexity of post-surgical knee pain and are familiar with the full range of treatment options available. This may require consulting with specialists such as interventional radiologists, pain management physicians, or orthopedic surgeons who have experience with complex cases.
Taking Action: Steps for Patients
Seek Specialized Evaluation
Patients with persistent pain after knee replacement should seek evaluation from specialists who have experience with this condition. This may include interventional radiologists who perform GAE, pain management specialists, or orthopedic surgeons who specialize in complex knee problems.
A comprehensive evaluation should include a detailed history, physical examination, and appropriate imaging studies to identify the specific causes of persistent pain. This evaluation is crucial for determining which treatment approaches are most likely to be effective.
Research Treatment Options
Patients should educate themselves about the various treatment options available for persistent knee pain. This includes understanding both traditional treatments and newer approaches like GAE. Reliable sources of information include medical websites, peer-reviewed research articles, and discussions with healthcare providers.
Consider Multiple Opinions
For complex cases of persistent pain after knee replacement, it may be beneficial to seek multiple medical opinions. Different specialists may have different perspectives on the best treatment approach, and patients can benefit from this diverse input when making treatment decisions.
Maintain Realistic Expectations
While effective treatments are available, it’s important for patients to maintain realistic expectations about outcomes. Complete elimination of pain may not always be possible, but significant improvement in pain and function is often achievable with appropriate treatment.
The Role of Healthcare Providers
Staying Current with Treatment Options
Healthcare providers who treat patients with knee problems should stay current with emerging treatment options like GAE. This includes understanding the indications for these procedures, the expected outcomes, and how to refer patients to appropriate specialists.
Multidisciplinary Approach
Complex cases of persistent pain after knee replacement often benefit from a multidisciplinary approach involving multiple specialists. Orthopedic surgeons, interventional radiologists, pain management specialists, and other healthcare providers should work together to develop comprehensive treatment plans.
Patient Education and Support
Healthcare providers play a crucial role in educating patients about their condition and treatment options. This includes helping patients understand the causes of their pain, the rationale for different treatments, and what to expect from various procedures.
Future Directions and Research
Ongoing Research
Research into GAE and other treatments for persistent knee pain continues to evolve. Ongoing studies are investigating optimal patient selection criteria, technique refinements, and long-term outcomes. This research will help improve the effectiveness of GAE and expand its applications.
Combination Therapies
Future research may explore the use of GAE in combination with other treatments to maximize effectiveness. This could include combining GAE with nerve blocks, physical therapy protocols, or other interventional procedures.
Personalized Medicine
As our understanding of the causes of persistent knee pain improves, treatment approaches may become more personalized based on individual patient characteristics. This could include genetic factors, inflammatory markers, or other biomarkers that help predict which treatments are most likely to be effective for each patient.
Conclusion: A New Chapter in Knee Pain Management
The journey of persistent pain after knee replacement surgery can be frustrating and disheartening, but it’s important for patients to know that they are not alone and that effective treatment options are available. The development of Genicular Artery Embolization represents a significant advancement in the treatment of knee pain, offering new hope for patients who have not found relief with traditional approaches.
GAE’s ability to target the underlying inflammatory processes that contribute to persistent pain makes it a valuable addition to the treatment armamentarium for post-surgical knee pain. Its minimally invasive nature, excellent safety profile, and proven effectiveness make it an attractive option for many patients who are seeking alternatives to revision surgery or long-term pain medication use.
For patients experiencing persistent pain after knee replacement, the key is to work with knowledgeable healthcare providers who can perform a comprehensive evaluation and discuss all available treatment options. This may include traditional approaches such as medications and physical therapy, as well as newer interventional procedures like GAE.
The future of knee pain management continues to evolve, with ongoing research leading to better understanding of pain mechanisms and more effective treatments. Patients who are struggling with persistent pain should not lose hope – effective treatments are available, and new options continue to emerge.
By staying informed about treatment options, working with experienced healthcare providers, and maintaining realistic but optimistic expectations, patients with persistent knee pain can look forward to improved function and quality of life. GAE represents just one example of how medical innovation can provide new solutions for challenging clinical problems, offering hope and healing for those who need it most.
References
[1] Wylde V, Beswick A, Bruce J, Blom A, Howells N, Gooberman-Hill R. Chronic pain after total knee arthroplasty. EFORT Open Rev. 2018;3:461-470. https://pmc.ncbi.nlm.nih.gov/articles/PMC6134884/
[2] International Association for the Study of Pain. IASP Terminology. Available at: https://www.iasp-pain.org/resources/terminology/
[3] Macrae WA. Chronic post-surgical pain: 10 years on. Br J Anaesth. 2008;101:77-86.
[4] Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2:e000435.
[5] Wylde V, Hewlett S, Learmonth ID, Dieppe P. Persistent pain after joint replacement: prevalence, sensory qualities, and postoperative determinants. Pain. 2011;152:566-572.
[6] Kurien T, Arendt-Nielsen L, Petersen KK, Graven-Nielsen T, Scammell BE. Preoperative neuropathic pain-like symptoms and central pain mechanisms in knee osteoarthritis predicts poor outcome 6 months after total knee replacement surgery. J Pain. 2018;19:1329-1341.
[7] National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. 19th Annual Report 2022. Available at: https://www.njrcentre.org.uk/
[8] Wylde V, Lenguerrand E, Gooberman-Hill R, et al. Effect of local anaesthetic infiltration on chronic postsurgical pain after total hip and knee replacement: the APEX randomised controlled trials. Pain. 2015;156:1161-1170.
[9] Singh JA, Lewallen DG. Depression in primary TKA and higher medical comorbidities in revision TKA are associated with suboptimal subjective improvement in knee function. BMC Musculoskelet Disord. 2014;15:127.
[10] Wylde V, Dieppe P, Hewlett S, Learmonth ID. Total knee replacement: is it really an effective procedure for all? Knee. 2007;14:417-423.
[11] Phillips CJ. The Cost and Burden of Chronic Pain. Rev Pain. 2009;3:2-5.
[12] Li CY, Karmakar MK, Li JW, Kwok WH, Kee WDN. Literature review of the causes of pain following total knee replacement surgery. Knee Surg Relat Res. 2020;32:41.
[13] Luo D, Yu L, Feng Y, et al. Chronic post-surgical pain after total knee arthroplasty: a systematic review and meta-analysis. Perioper Med (Lond). 2024;13:66.
[14] Li CY, Karmakar MK, Li JW, Kwok WH, Kee WDN. Literature review of the causes of pain following total knee replacement surgery. Knee Surg Relat Res. 2020;32:41. https://pmc.ncbi.nlm.nih.gov/articles/PMC7528670/
[15] Sugimura N, Iwamoto N, Fukui S, et al. Temporal changes in synovitis and chronic pain after total knee arthroplasty. Osteoarthr Cartil Open. 2025;7:100506.
[16] Gandhi R, Santone D, Takahashi M, Dessouki O, Mahomed NN. Inflammatory predictors of ongoing pain 2 years following knee replacement surgery. Knee. 2013;20:316-318.
[17] Taslakian B, Miller LE, Mabud TS, et al. Genicular artery embolization for treatment of knee osteoarthritis pain: Systematic review and meta-analysis. Osteoarthr Cartil Open. 2023;5:100342. https://pmc.ncbi.nlm.nih.gov/articles/PMC9971280/
[18] Taslakian B, Miller LE, Mabud TS, et al. Genicular artery embolization for treatment of knee osteoarthritis pain: Systematic review and meta-analysis. Osteoarthr Cartil Open. 2023;5:100342.
[19] Bagla S, Rholl KS, van Breda A, Sterling KM, van Breda A. Geniculate artery embolization in the management of spontaneous osteonecrosis of the knee. Cardiovasc Intervent Radiol. 2013;36:123-127.
This article is for educational purposes only and should not replace professional medical advice. Patients experiencing persistent pain after knee replacement surgery should consult with qualified healthcare providers to discuss their individual situation and treatment options.
About ARV CentersARV Centers specializes in advanced interventional radiology procedures, including Genicular Artery Embolization for knee pain. Our team of experienced interventional radiologists is dedicated to providing innovative, minimally invasive treatments for patients with complex pain conditions. For more information about GAE and other treatment options, contact ARV Centers to schedule a consultation.
- Lindsey’s LIFE-CHANGING Non-Surgical Fibroid Treatment Experience!
- Still Hurting After Knee Replacement? What to Do When the Pain Persists
- Beyond the Scalpel: A Minimally Invasive Approach to Hemorrhoid Relief – Understanding Your Options
- Navigating BPH Treatment: From Lifestyle Changes and Medications to Advanced PAE – What Are Your Options?
- Knee Arthritis: What Your Orthopedic Surgeon May Not Be Telling You