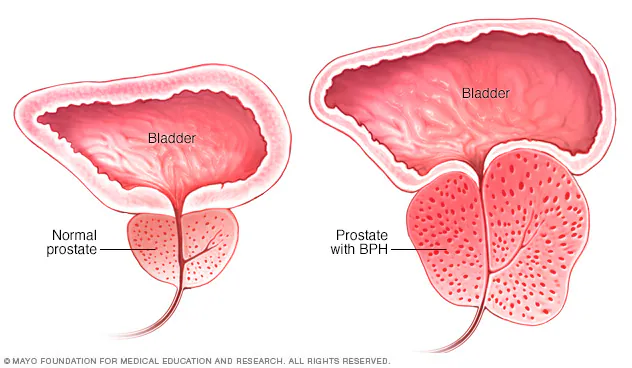
Benign Prostatic Hyperplasia (BPH), commonly known as an enlarged prostate, affects a vast number of men as they age, leading to bothersome urinary symptoms that can significantly impact quality of life. If you’re experiencing issues like frequent urination, a weak stream, or an urgent need to go, you’re not alone. Fortunately, various treatment options are available, ranging from lifestyle changes and natural approaches to advanced minimally invasive procedures.
At Arthritis Relief & Vascular Centers (ARVC), we believe in empowering patients with knowledge. This post will compare and contrast different approaches for treating BPH, with a special focus on a highly effective, minimally invasive option we offer: Prostatic Artery Embolization (PAE).
Understanding BPH and Its Symptoms
BPH is a non-cancerous enlargement of the prostate gland, a small gland located below the bladder in men. As the prostate grows, it can squeeze the urethra, the tube that carries urine from the bladder, leading to Lower Urinary Tract Symptoms (LUTS) such as:
- Frequent or urgent need to urinate
- Increased urination at night (nocturia)
- Difficulty starting urination
- Weak or interrupted urine stream
- Dribbling at the end of urination
- Inability to completely empty the bladder
If these symptoms sound familiar, it’s essential to consult a healthcare professional for an accurate diagnosis.
A Spectrum of BPH Treatment Approaches
Choosing the right BPH treatment depends on several factors, including the severity of your symptoms, prostate size, overall health, and personal preferences. Here’s an overview:
1. Watchful Waiting, Lifestyle Modifications & Natural Approaches
- Description: For men with mild symptoms that aren’t particularly bothersome, a “watchful waiting” approach may be suitable. This involves regular monitoring by a physician. Lifestyle adjustments and natural approaches can also help manage symptoms.
- Examples:
- Limiting fluids before bed (especially caffeine and alcohol).
- Dietary changes: Reducing spicy foods, red meat; increasing fruits and vegetables. Eating red fruits like tomatoes and watermelon, which are rich in lycopene, may offer some prostate health benefits.
- Managing weight and engaging in regular physical activity.
- Bladder training and pelvic floor exercises (Kegels) can help improve bladder control and manage urgency.
- Reducing stress.
- Pros: Non-invasive, no medication side effects from lifestyle changes.
- Cons: May not be sufficient for moderate to severe symptoms; BPH can progress. Natural remedies have limited scientific evidence for significant BPH reversal but can support overall prostate health and symptom management.
- Examples:
2. Medications
- Description: This is often the first line of treatment for mild to moderate BPH.
- Types & How They Work:
- Alpha-blockers (e.g., Tamsulosin, Alfuzosin): Relax the muscles in the prostate and bladder neck, making urination easier.
- 5-alpha reductase inhibitors (e.g., Finasteride, Dutasteride): Shrink the prostate by preventing hormonal changes that cause prostate growth.
- Combination Therapy: Using both types of medication together.
- Tadalafil (Cialis): Also used for erectile dysfunction, it can help relieve BPH symptoms.
- Pros: Non-surgical, can be effective for symptom relief.
- Cons: Potential side effects (dizziness, retrograde ejaculation with alpha-blockers; sexual side effects with 5-alpha reductase inhibitors), ongoing medication cost, may not be effective for all men or for very large prostates. Additionally, some men experience “medication fatigue” or issues with long-term compliance (non-compliance) with daily medication regimens.
- Types & How They Work:
3. Minimally Invasive Surgical Therapies (MIST)
- Description: These are newer procedures that aim to relieve BPH symptoms with less risk and shorter recovery times than traditional surgery. They are typically performed by urologists.
- Rezum (Water Vapor Thermal Therapy):
- How it works: Uses sterile water vapor (steam) to ablate (destroy) targeted prostate tissue that is causing obstruction.
- Pros: Can be effective for various prostate sizes, outpatient procedure.
- Cons: Can be incredibly painful post-procedure due to the prostate heating with steam. Recovery can involve a period of swelling and irritation, often requiring a temporary catheter. Generally does not preserve sexual function as well as UroLift or PAE for some patients, with some reporting changes in ejaculation.
- UroLift (Prostatic Uthral Lift):
- How it works: Small, permanent implants are used to lift and hold the enlarged prostate tissue away from the urethra, opening the urinary channel. No cutting, heating, or removal of prostate tissue.
- Pros: Rapid symptom relief for many, generally good preservation of sexual function (low rates of new, sustained erectile or ejaculatory dysfunction), can often be done under local anesthesia.
- Cons: The UroLift system utilizes permanent implants. While these are made of standard implantable materials, their permanent nature can potentially limit or complicate future BPH treatment options if needed, as removing the implants can be challenging. It also has a relatively high retreatment rate compared to some other procedures, meaning some men may need additional BPH treatment later on. Not always ideal for all prostate shapes, such as those with a large obstructive median lobe.
- Rezum (Water Vapor Thermal Therapy):

Traditional Surgical Procedures
- alteration of prostate tissue. They have long been considered for more significant BPH when other treatments are insufficient or unsuitable, and are typically performed by urologists.
- Transurethral Resection of the Prostate (TURP):
- How it works: A surgeon inserts a resectoscope (a thin instrument with a light, camera, and electrical loop) through the urethra to the prostate. The heated electrical loop is then used to cut away and remove obstructing prostate tissue piece by piece.
- Pros: Has been considered a “gold standard” for many years due to its effectiveness in relieving symptoms for a significant duration. Provides tissue for pathological examination.
- Cons: Requires general or spinal anesthesia and typically a hospital stay of 1-3 days. A urinary catheter is needed for a period post-surgery. TURP is generally most suitable for small to moderately sized prostates (often cited up to 80-100 grams); for very large glands, the procedure time can become excessively long, increasing risks, or it may not be feasible to remove enough tissue in a single session. Key risks include bleeding (which can sometimes require transfusion), infection, TUR syndrome (a rare but serious metabolic complication from absorption of irrigation fluid, though less common with newer bipolar TURP techniques), urinary incontinence (usually temporary but can be persistent), urethral strictures (scarring), and a high rate of retrograde ejaculation (dry orgasm) where semen enters the bladder instead of being ejaculated. Erectile dysfunction can also occur in a percentage of patients.
- Holmium Laser Enucleation of the Prostate (HoLEP):
- How it works: A high-powered holmium laser is delivered through a scope inserted into the urethra. The laser is used to precisely cut out and separate the enlarged portion of the prostate (the adenoma) from its outer capsule. The removed tissue is then pushed into the bladder and suctioned out using a morcellator.
- Pros: Highly effective for relieving symptoms, even for very large prostates, often considered an endoscopic equivalent to open prostatectomy. Results are durable with a low re-treatment rate. Offers a low risk of significant bleeding, making it suitable for patients on blood thinners. Removed tissue is available for pathological examination. Typically involves a shorter hospital stay and catheterization time compared to TURP or open surgery.
- Cons: Requires general or spinal anesthesia. Has a steeper learning curve for surgeons. Common temporary side effects include burning during urination, urinary frequency/urgency, and some blood in the urine, which can last for several weeks. Retrograde ejaculation is a very common and expected side effect. Temporary stress incontinence or urge incontinence can occur while the bladder and sphincter muscles recover and re-strengthen.
- GreenLight™ Laser Therapy (Photoselective Vaporization of the Prostate – PVP):
- How it works: A laser fiber is passed through a scope into the urethra. High-powered laser energy is then used to heat and vaporize the obstructing prostate tissue, creating an open channel for urine flow.
- Pros: Generally results in less bleeding than TURP, often allowing for a shorter hospital stay (sometimes outpatient) and shorter catheterization time. Can be a good option for patients on certain anticoagulant medications.
- Cons: Requires anesthesia. May cause irritative urinary symptoms (burning, frequency, urgency) for a period after the procedure as the area heals. Retrograde ejaculation is a common side effect, though its incidence might be slightly lower than with TURP or HoLEP in some studies. The effectiveness for very large prostates might be limited compared to HoLEP or open surgery, as completely vaporizing large volumes of tissue can be lengthy and challenging. Since the tissue is vaporized, it is not available for pathological analysis.
- Open Prostatectomy (Simple Prostatectomy – nowadays often robot-assisted):
- How it works: This is the most invasive traditional surgical option, generally reserved for men with very large prostates (often >80-100 grams) or when there are other complicating factors like large bladder stones or diverticula that need to be addressed simultaneously. The surgeon makes an incision in the lower abdomen (for the open approach) or several small incisions (for the laparoscopic/robotic approach) to access and remove the inner core of the enlarged prostate that is causing the blockage.
- Pros: Considered the most effective procedure for removing large amounts of prostate tissue and providing significant, long-lasting symptom relief, especially for men with very large glands.
- Cons: Carries the highest risk of complications among BPH surgeries, including significant bleeding (potentially requiring transfusion) and infection. Involves the longest hospital stay and the most extended recovery period (often several weeks to months). A urinary catheter is required for a longer duration post-surgery. Higher risks of urinary incontinence (both stress and urge) and erectile dysfunction compared to less invasive methods. Retrograde ejaculation is an almost certain outcome.
- Transurethral Resection of the Prostate (TURP):
Introducing Prostatic Artery Embolization (PAE) – An Advanced, FDA-Approved Solution at ARVC
At Arthritis Relief & Vascular Centers, we are proud to offer Prostatic Artery Embolization (PAE), an advanced, FDA-approved, minimally invasive treatment for BPH performed by our skilled Interventional Radiologists. It’s important to note that PAE is also listed in the American Urological Association (AUA) Guidelines as a treatment option for BPH, highlighting its recognized efficacy and safety.
- What is PAE? PAE is a non-surgical procedure that works by reducing the blood supply to the enlarged prostate gland. An Interventional Radiologist makes a tiny incision, usually in the wrist or groin, and guides a very small catheter through the arteries to the vessels supplying the prostate. Microscopic, medical-grade beads are then injected, blocking these specific arteries. This deprivation of blood flow causes the prostate to soften and shrink over time, relieving pressure on the urethra and alleviating urinary symptoms.
- Who is a Good Candidate for PAE? PAE is an excellent option for men with moderate to severe BPH symptoms who:
- Have not found adequate relief with medications or are experiencing medication fatigue.
- Wish to avoid the risks and side effects of traditional surgery or other MIST procedures.
- May not be good candidates for surgery due to other medical conditions.
- Want to preserve sexual function.
- Have larger prostates, where some other MIST procedures may be less effective or suitable.
Key Benefits of Prostatic Artery Embolization (PAE) at ARVC:
- Minimally Invasive: No large incisions, performed through a tiny puncture.
- Outpatient Procedure: Patients typically go home the same day.
- Significant Symptom Improvement: Leads to noticeable improvements in urine flow, frequency, urgency, and nocturia.
- Preservation of Sexual Function: PAE has a very low risk of causing erectile dysfunction or retrograde ejaculation.
- Low Risk of Urinary Incontinence.
- Quick Recovery: Most men can return to normal activities within a few days.
- No General Anesthesia Required: Typically performed under local anesthesia and mild “twilight” sedation.
- Effective for Various Prostate Sizes.
- No Permanent Implants Left Behind: Unlike some other MIST procedures.
Making the Right Choice for Your BPH
The journey to BPH relief is personal. While lifestyle changes, natural approaches, and medications can be effective for some, others may require more definitive treatment. Minimally invasive options like PAE present an outstanding balance of efficacy, safety, and preservation of quality of life, especially when compared to more invasive surgeries or procedures with permanent implants or higher risks of sexual side effects.
Why Consider ARVC for Your PAE Procedure?
At Arthritis Relief & Vascular Centers, our team of experienced Interventional Radiologists specializes in advanced, image-guided procedures like PAE. We are committed to providing personalized care, utilizing the latest techniques to ensure the best possible outcomes for our patients.
Take the Next Step Towards BPH Relief
If you are struggling with the symptoms of BPH and are interested in learning more about Prostatic Artery Embolization (PAE) as an FDA-approved, AUA-recognized, minimally invasive treatment option, we invite you to schedule a consultation with our specialists.
- Call Arthritis Relief & Vascular Centers today at 210-899-0384
- Visit our website at www.arvcenters.com to learn more or to request an appointment.
Don’t let BPH control your life. Explore your options and find the path to lasting relief.